There are huge differences in the mortality rate (COVID-19) and toll due to coronavirus disease 2019. This is likely to be due to socio-demographic, climatic or other factors. However, it is possible that there are additional factors that contribute to the variation in disease outcomes at local levels.
These factors can be used to predict the trajectories for pandemics. This may help with non-pharmaceutical interventions as well as research directions for the development of new therapeutic and immunological strategies.
Interactions between the host and non-pathogenic microbes can also have a significant impact on disease outcomes, such as those of COVID-19.
The following features are common to environmental microbes that promote health outcomes:
- Environmental microbes having beneficial effects often originate from soils, freshwater environments, plants, and other non-anthropogenic sources – potentially reflecting a history of human evolutionary adaptation to them
- These microbes can reduce the severity of diseases by stimulating the immune systems early in life.
- It is important to be exposed to diverse microbes to achieve beneficial effects
Functional immune response is essential for moderating outcomes of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. In addition, evidence suggests that COVID-19 disease severity correlates with bacterial community composition in patients and the hospital environment and with dysbiosis of the lung and the gut microbiomes.
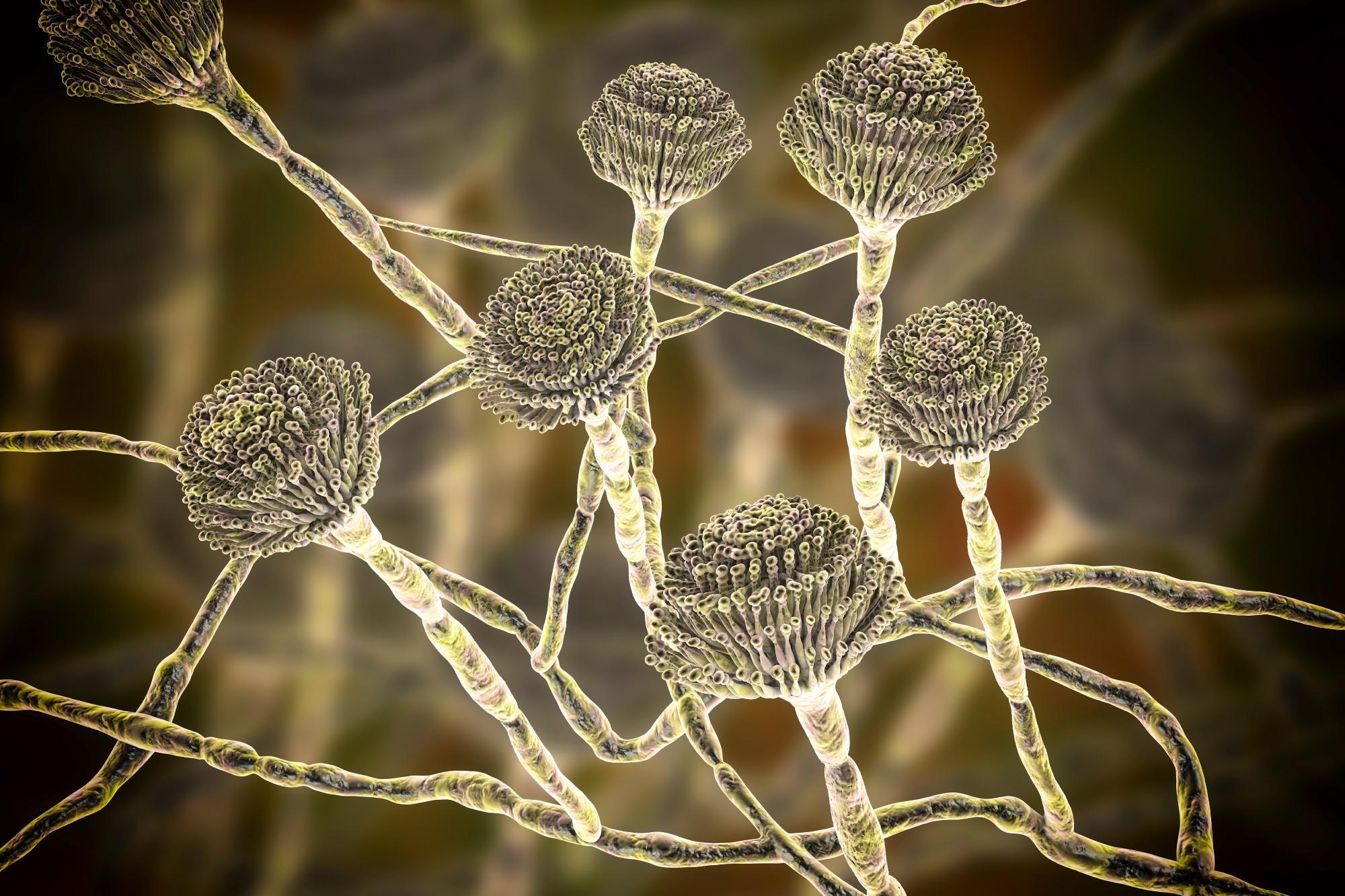
A new study published on the medRxiv* preprint server was based on the hypothesis that the environmental mycobiome (fungi) is a likely important factor in determining area-level variation in COVID-19 mortality.
 PIN IT
PIN IT
The study
The present study utilized taxonomic information on fungal communities from 1,135 homes nationwide, as well as COVID-19 data from across the United States. Paired samples were collected from each house—indoors and outdoors—allowing for comparison. An innovative approach was used to estimate the number of SARS-CoV-2 deaths per 1,000 infections in each county in the United States and in each home which provided fungal data.
Additionally, the influence of demographic, sociological, climate and soil factors was extensively explored, some of which influence Infection Fatality Ratios (IFR) and fungal community composition.
Findings
It was noted that a majority of the citizens primarily interact with indoor microbes only—as they spend most of their time in their homes or other constructed environments. For fungi, two major types were of concern – non-pathogenic outdoor species (which are sometimes also found indoors) and pathogenic or opportunistic species that proliferate in damp indoor environments. These types elicited notable differences.
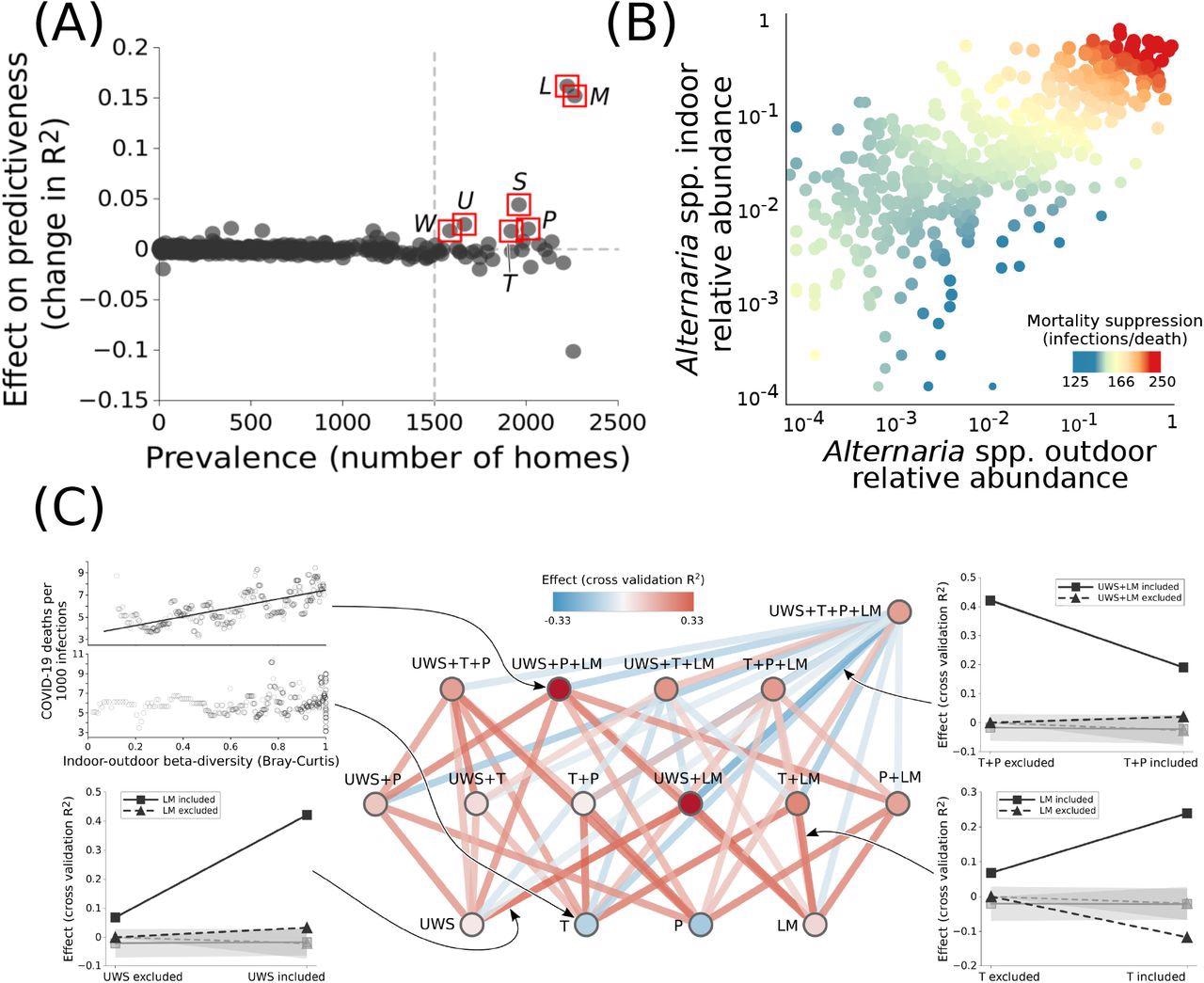
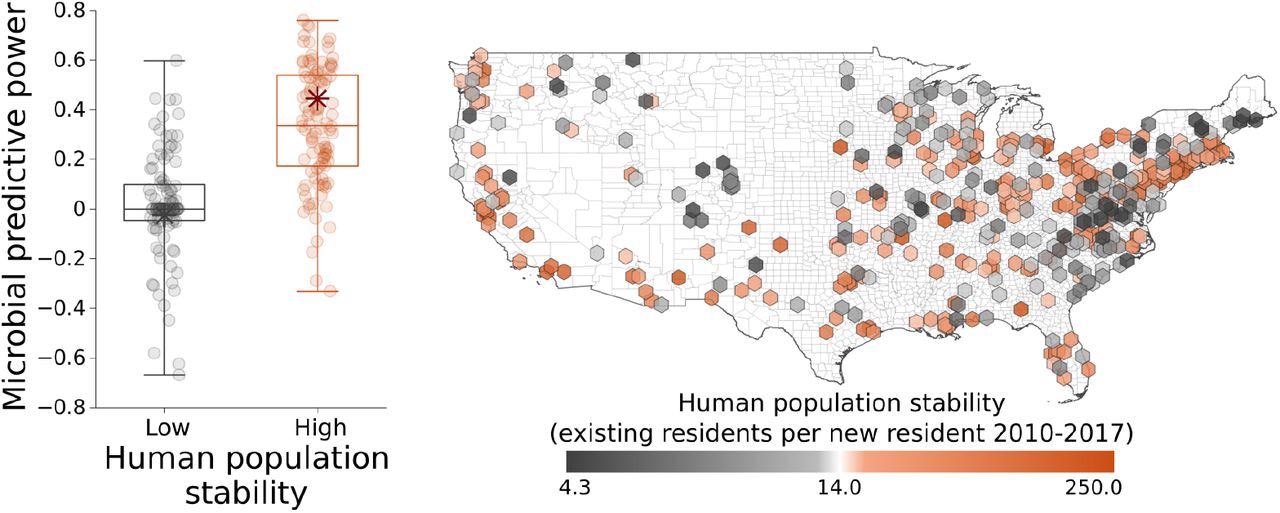
SARS-CoV-2 IFR was reduced by the presence of outdoor fungal genera in the built environment. Based on the analysis, a marginal impact was observed of the relative abundances of fungal genera or indoor-outdoor beta diversity—after taking into account demographic, sociological, climate and soil factors. The relative abundances for fungal genera had a statistically significant, but very small effect on the mean IFR when considering all the other factors.
Quantile analysis revealed that indoor/outdoor beta-diversity was associated with lower SARS-2 IFR, which indicates decreased mortality. However, it was found that indoor-outdoor mycological flora is associated with higher SARS-CoV-2IFR. These results were consistent across all counties.
The presence of indoor fungi with high diversity was associated with lower COVID-19 deaths than indoor fungi. This association was valid in the first few months of the pandemic and weaker during the later phases—December 2020 to January 2021—after vaccine availability and in the setting of access to pharmaceutical treatments.
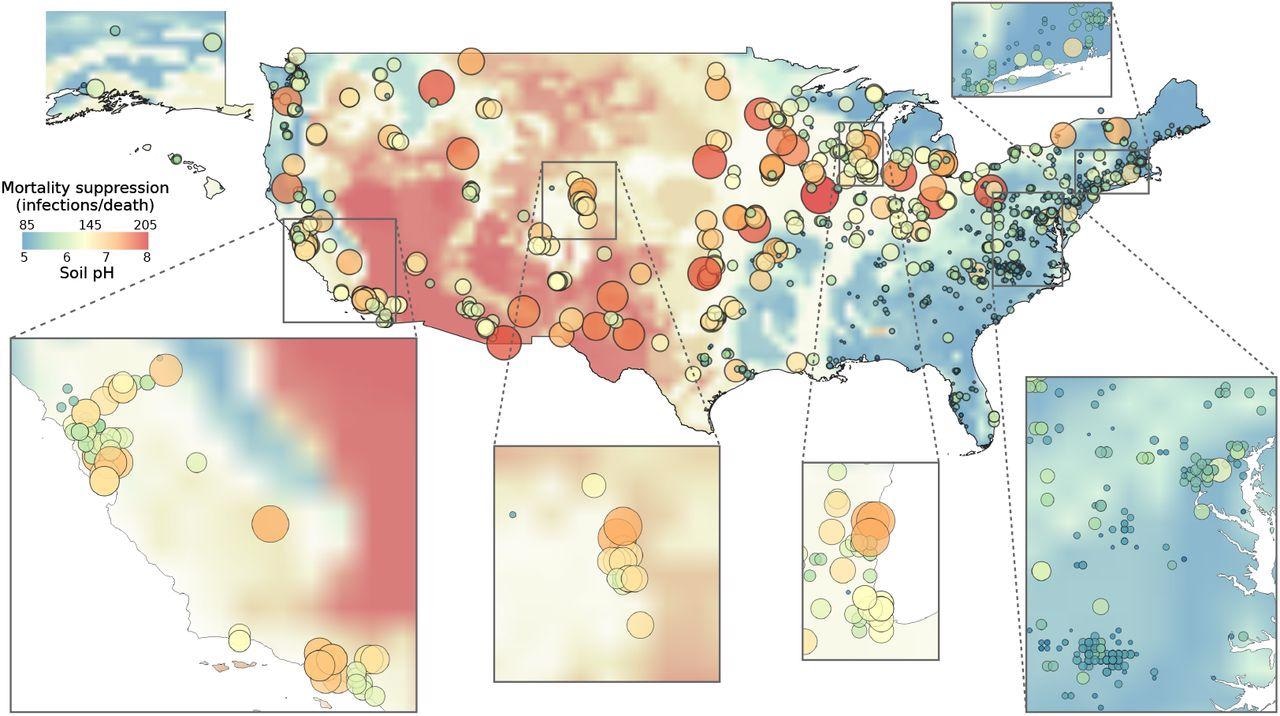
Remarkably, soil edaphic factors – particularly pH, appeared to affect COVID-19 severity by affecting microbial distributions. A causal link was also found between indoor-outdoor fungal beta diversity and SARS-CoV-2IFR, even after considering other variables.
The results revealed that at least four of these fungal genera play a key role in suppressing SARS-CoV-2 IFR, which are – Alternaria, Aspergillus, Epicoccum, Eurotium, Toxicocladosporium, Wallemia spp., Novel Mycosphaerellaceae genus. Some of these have interdependent occurrences. It is therefore difficult to determine the effects of individual genera. For significant SARS-CoV-2 IFR decrease, it is important to have three of these genera in high relative abundance both indoors as well as outdoors.
These findings are a new illustration of the positive effects of seven mycological genises on COVID-19 mortality. These genera can be pathogenic in some environments, but they may have positive effects on others.
Additionally, different species of endemic and environmental microbes can have different effects depending on host genetics, age, immune status and interactions with other microbial exposures.
Positive synergistic effects were identified among the seven genera studied in this study. This makes it possible to predict how their beta-diversity will affect each other. Fungal beta diversity was also strongly associated with SARS/CoV-2 IFR suppression in areas with stable human habitation. Hence, these observations could accurately map locations to forecast regions with strong suppression of COVID-19 mortality in the US – the Desert Southwest, Intermountain West, and Upper Midwest.
pH, in addition to the US climate, may indicate the microbial composition of the US and the propensity for microbial transportation into homes via dust. There is a correlation between bioaerosol counts and incidence of respiratory diseases.
In conclusion, high levels of outdoor fungal species in your home can protect you from poor COVID-19 outcomes. These results highlight the utility of the environment mycobiome as an indicator. The beneficial effects of environmental mushrooms may not only be applicable to COVID-19, but may also be applicable to other immune-mediated and autoimmune diseases.
Further research is needed to understand the role of fungal interactions with the host immune systems and the role they play in this process. Recent advancements in the classification and sequencing of environmental fungi will improve future efforts and highlight the utility of biosurveillance in future pandemics.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Ladau, J., Abuabara, K., Walker, A., et al. (2021), “The impact of environmental microbiomes on geographic variation in COVID-19 mortality”, medRxiv preprint, doi: 10.1101/2021.12.14.21267549, https://www.medrxiv.org/content/10.1101/2021.12.14.21267549v1