[ad_1]

This is a collaboration between Public Health Watch and the Investigative Reporting Workshop.
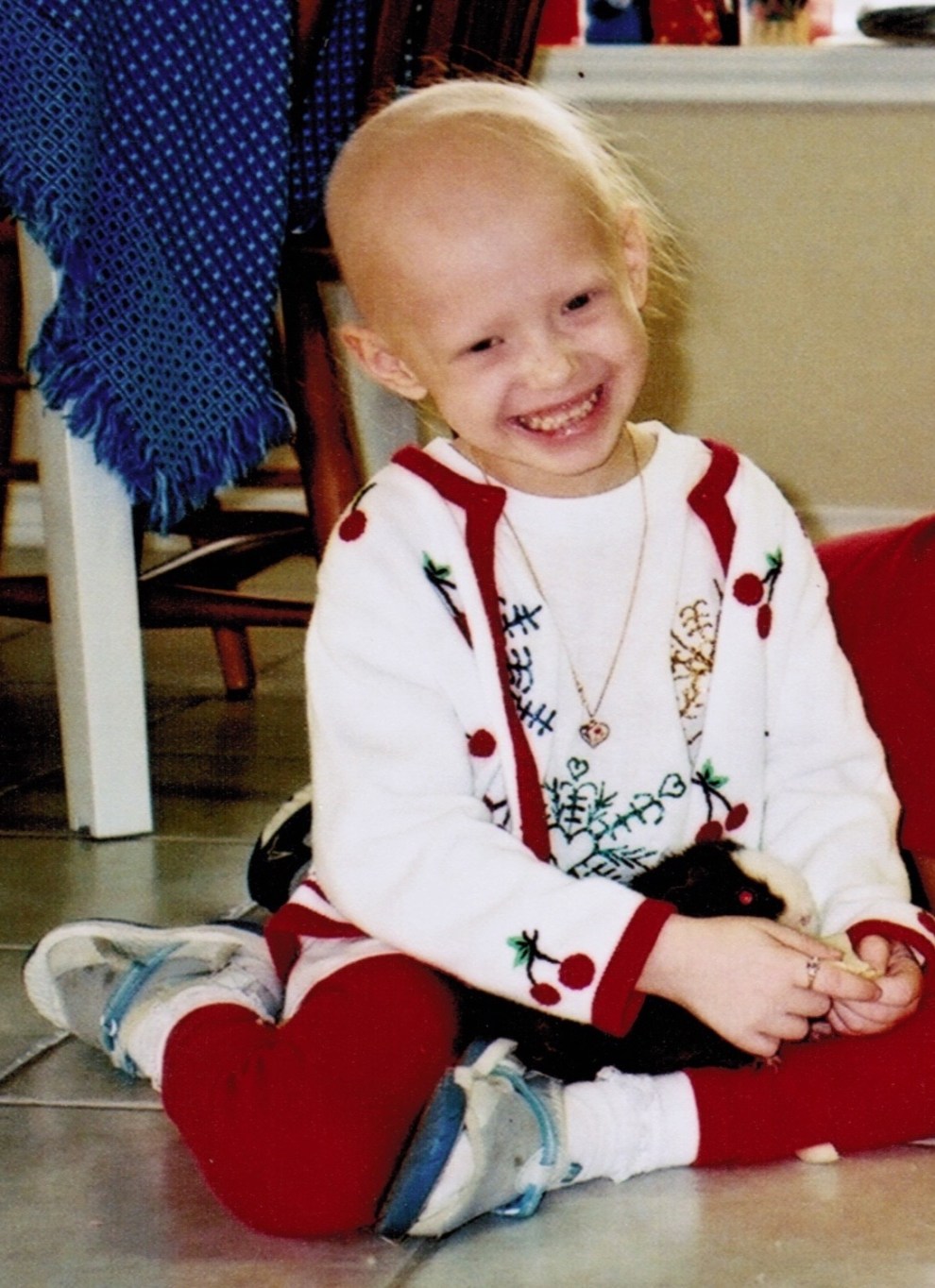
In April 2008, Jonathan Agin’s 27-month-old daughter, Alexis, was diagnosed with DIPG, a rare brain tumor. Agin, then a civil defense lawyer in Washington, DC, was dislodged from his comfortable life and dragged into the surreal world of a young cancer victim’s parent: The sleepless nights in the din of a hospital, the grueling clinical trials.
“I always had hope,” Agin said in a recent interview, though he knew most DIPG patients survive no more than two years after diagnosis.
Alexis lived for 33 months after her tumor was found. Toward the end of her life, she was unable to walk or speak. She died at 3:03 p.m. on Jan. 14, 2011.
“My knowledge back then of children with cancer was watching St. Jude and Ronald McDonald House commercials,” Agin said. The image of a “smiling, bald-headed kid living happily ever after” was cruelly misleading, he learned, when it came to intractable cancers like DIPG, short for Diffuse Intrinsic Pontine Glioma.

Alexis.
(Photo courtesy Jonathan Agin)
While children with a diagnosis like Alexis face almost insurmountable odds, death rates for many childhood cancers have gone down, thanks to advances in treatment. But incidence rates—the number of cancer cases per 100,000 children—increased 43 percent from 1975 to 2018. While there’s no clear explanation, some experts suspect environmental contamination has played a major role.
“These increases are too rapid to be due to genetic change,” pediatrician Philip Landrigan wrote in a report last year for the Childhood Cancer Prevention Initiative, a collaborative that includes the Children’s Environmental Health Network, the American Sustainable Business Council, and other organizations.
“They cannot be explained by increased access to medical care or by improvements in diagnosis,” wrote Landrigan, director of the Program for Global Public HealthThe Common Good at Boston College. His theory is that exposure in the womb or early childhood to chemicals is driving the trend. “Recognition is growing that hazardous exposures in the environment are powerful causes of cancer in children,” he wrote.
When it comes to drug development, children with cancer—defined as people under the age of 20—have long been at the back of the line. There simply aren’t enough of them to inspire massive investment. In 2018, most recent year for which complete data is available, 15,178 children in the United States were diagnosed with cancer and 1,841 died, according to the Centers for Disease Control and Prevention. In comparison, 599 265 adults were also affected and 599 265 died.
It is now clear that some of the 86,000 chemicals used in the United States may have a significant impact on children. Safety testing has not been done on many of these chemicals.
“The American public loves treatments, loves magic fixes,” Landrigan said in an interview. “The rising incidence is not a good-news story. There are no heroes.”
April 2010,The President’s Cancer PanelRichard Nixon established the advisory group, ‘the ‘Advisory Group’, in 1971. groundbreaking report highlighting what it called the “growing body of evidence linking environmental exposures to cancer.”
The panel concluded that “the true burden of environmentally induced cancer has been grossly underestimated. With nearly 80,000 chemicals on the market in the United States, many of which are used by millions of Americans in their daily lives and are un- or understudied and largely unregulated, exposure to potential environmental carcinogens is widespread….The American people—even before they are born—are bombarded continually with myriad combinations of these dangerous exposures.”
Dr. Margaret Kripke was a co-author of this report. She founded and chairs the Department of Immunology at The University of Texas. Anderson Cancer Center, Houston. Kripke, now retired, stated that the panel had already considered lifestyle factors such as smoking and nutrition, but it turned its attention to the environment due to public interest in the topic.
“I was not that enthusiastic about this in the beginning,” she said. “It was controversial, unclear what we’d advise the public to do.”
Kripke’s opinion changed as she worked on the report in 2008 and 2009. “It was truly the most eye-opening experience for me,” she said. “I learned how little attention had been paid to this issue for a very long time.”
That inattention comes in part because “childhood cancers still make up only 1 percent of the cancer diagnoses in the US,” said Dr. Philip Lupo, an associate professor at Baylor College of Medicine in Houston and a genetic epidemiologist at Texas Children’s Cancer and Hematology Center. “That creates a challenge for epidemiologists, who often need large sample sizes.”
Lupo and Dr. Michael Scheurer (a Baylor colleague) have begun collecting biological samples, such as saliva samples, from newly diagnosed patients. Then, they gave questionnaires their parents to determine if there are any risk factors for developing breast cancer.
“As we see this explosion in environmental chemicals in human populations, it’s entirely likely they’re playing an important role in the increased incidence of childhood cancer,” Lupo said. Some, such as benzene (a solvent and gasoline ingredient), have been shown in animal and occupational studies to cause DNA destruction, which is a precursor for the disease.
It’s unlikely genetics are behind the rising numbers, Lupo said, “because genetics don’t work that quickly.”
Congress created a bodyAs part of the investigation, we will examine possible connections between chemical exposures to illness. Superfundlegislation in 1980. However, the Agency for Toxic Substances and Disease RegistryCDC has never gained widespread credibility for its part.
1992 saw the release of a document by the Environmental Health Network (now the National Toxics Campaign Fund) report accusing the agency of conducting poorly designed studies “used by polluters and government officials to mislead local citizens into believing that further measures to prevent toxic exposures are unnecessary.”
Stephen Lester, science Director at the Center for Health, Environment and Justice, is a research and advocacy group in suburban Washington, DC. The disease registry, known as the ATSDR, relies on existing data—generated, for example, by a state environmental agency—that is often incomplete and of little value for assessing health risks.
“The conclusions are always limited by the data,” Lester said. “Even if the agency could determine that a health cluster exists—and I’ve seen them do that maybe two times out of hundreds of cases—they cannot determine what’s causing the cluster.”
In an emailed statement to Public Health Watch and the Investigative Reporting Workshop, the CDC said, “While we know that chemical exposures can contribute to a variety of health issues and we continue to learn more about these pathways, determining a causal relationship from community-based chemical exposures to specific cases of cancer is rare.”
The ATSDR is being stretched thin, having seen its “purchasing power eroded by relatively flat funding levels despite increasing demand for support in responding to environmental exposures,” the statement said.
In recent years, Congress provided $4.5 million to the agency to help it update its website. guidelinesTo study cancer clusters. The money came from the Strengthening Protections for Children and Communities from Disease Clusters Act—better known as Trevor’s Law, after Trevor Schaefer, who was diagnosed with medulloblastoma, a form of brain cancer, when he was 13 and living in McCall, Idaho, a small town north of Boise.

Schaefer and his mother, Charlie Smith, believe his illness was triggered by waste from an abandoned mine that wound up in the lake that supplied McCall’s drinking water. Five children in the town of 1,700 developed brain cancer within nine months of Schaefer’s diagnosis in 2002, but state health authorities said they found no evidence of a cluster.
Smith won the ear of then-Senator Barbara Boxer, D-California, who introduced Trevor’s Law in 2011. The bill was stalled and was finally signed into law in 2016 by President Barack Obama. Schaefer said he’s grown increasingly impatient with the ATSDR’s failure to finish updating the guidelines in the five years since.
“While the federal government drags its feet and fritters away essential funding, our children are dying,” he wrote in an email to Public Health Watch.
The CDC stated that it used the funds to review scientific literature, convene a scientific panel to discuss best practices and meet with community members to address their concerns.
“Concurrent with efforts to update the guidelines are projects aimed at making county-level cancer rate data more readily available and a pilot effort to determine the utility of electronic health records to provide more timely cancer surveillance data,” the agency said.
Schaefer, who runs The Schaefer Interview, talks about the interview. Trevor’s Trek Foundation, said, “We’re frustrated. When we talk to parents around the country, they’re getting frustrated. It doesn’t seem like it should take this long.”
In 1942, the Industrial Hygiene Foundation of America was founded presciently advised, “Every new chemical or product should be investigated as to its toxicity before it is prepared in large amounts and released to the public.” Twenty years later, in her book Silent SpringRachel Carson, a biologist warned about the dangers of pesticides like DDT. “If we are going to live so intimately with these chemicals, eating and drinking them, taking them into the very marrow of our bones—we had better know something about their nature and their power,” she wrote.
President John F. Kennedy listened to excerpts from the book. The New Yorker and was so shaken he established a special panel to investigate Carson’s dire predictions. The panel’s report in May 1963 validated Carson’s findings and bolstered her credibility, which had come under fierce attack by the chemical industry.
Silent SpringThis created momentum for the 1970 creation of the Environmental Protection Agency and the subsequent phaseout DDT. But the chemicals kept coming. 1976 was the year Congress passed the Toxic Substances Control Act More than 60,000 were available on the market when the TSCA was implemented to require safety testing. They were grandfathered in—assumed to be safe unless the EPA could demonstrate otherwise.
This proved to too much of a burden. The EPA has limited the use of a handful chemicals that were in commercial commerce before 1976. These include certain forms of asbestos, hexavalent chromium, dioxin contaminated wastes and paint-stripper methylenechide.
Congress amended TSCA in 2016 in part to shift the burden of proof from the EPA to chemical manufacturers to demonstrate new chemicals are unlikely to present “unreasonable” risks to human health or the environment before being allowed onto the market. However, the agency’s new-chemical reviews were undermined during the Trump administration by unrealistic assumptions that made chemicals appear safer than they actually were.
“Reviews of existing chemicals were also undermined by tenuous assumptions and illegal exclusions of certain sources of exposure, including environmental releases—of particular relevance to fenceline communities,” said Dr. Jennifer McPartland, a senior scientist with the Environmental Defense Fund.
Although the Biden Environmental Protection Agency (EPA) has attempted to repair the damage, they are still far behind. As of August, the agency’s TSCA inventory had climbed to 86,607 chemicals, 41,953 of which were considered “active”—manufactured or processed in recent years.
“EPA has to assess the risk of each and every one of those [active] chemicals, but it’s doing so at about 20-something a year,” McPartland said. Each risk evaluation is supposed to take 3 to 3 ½ years.
The math—nearly 42,000 chemicals and only 20 reviews a year—doesn’t bode well for public health.
“It’s the reality of a lack of regulation for decades,” McPartland said.
The EPA must also evaluate new chemicals before they can be put on the marketplace. Although the agency claims that it has completed 3,394 of these assessments, not all assessments result in a requirement for testing, McPartland stated that the program is also flawed. It’s needlessly opaque, she said, and its managers accede too often to companies’ demands for quick decisions.
In a June press releaseThe EPA stated that it had taken steps in order to strengthen risk evaluations on 10 high-priority chemicals, including 1,4-dioxane and methylene chloride. These chemicals are found in paints, detergents, and other products which have contaminated water in certain parts of the country. The agency said it would take into consideration “exposure pathways,” such as air and water, that had been disregarded by the Trump administration. The aim is to “restore public trust, provide regulatory certainty, and, most importantly, ensure that all populations that may be exposed to these chemicals are protected,” the EPA’s assistant administrator for the Office of Chemical Safety and Pollution Prevention, Michal Freedhoff, was quoted as saying.
In a written statement responding to questions from Public Health Watch and the Investigative Reporting Workshop, the EPA said it found “risks across many uses of these chemicals and will be proposing rules to protect against these risks beginning in 2022.” The agency said it has begun working on the next 20 evaluations.
The health impacts of cancer-causing chemicals land heaviest on low-income communities and communities of color, said Nsedu Obot Witherspoon, executive director of the Children’s Environmental Health Network. In such places “people who are doing all the right things—you know, taking care of their children the best they can and sending them to school and working hard”—face carcinogenic exposures from industrial facilities, heavily traveled highways, and other polluting sources.
Witherspoon was born in 1975 when childhood cancer incidence began to rise. “That shows you, right there, it’s not genetics only,” she said. “There’s something else happening that is making young, young children predisposed. Certain levels of exposure can lead to certain types of brain cancers, such as childhood leukemia, and whatnot. When you look at young children, they’re not smoking, they’re not drinking.”
Some in the private sector aren’t waiting for government intervention. Two students from the University of Texas were among those who attended the Helen R. Walton Children’s Enrichment CenterCancer was diagnosed in Bentonville, Arkansas. The illnesses were found to not be hereditary. Suspection was raised about chemicals the children might’ve ingested, inhaled or absorbed during their daily lives.
“It made us think twice about what we could be doing better,” said the center’s executive director, Michelle Barnes. “I was just horrified to hear about what is in our furnishings and carpets and things like sealants and non-stick cookware.”
The 1982 opening of the campus was already marked for replacement. After the students’ cancer diagnoses, Barnes, other members of the center’s leadership team, and its board of directors were determined to do things differently. New York-based LTL ArchitectsHe was found to have the right sensibility, and was hired in 2016. The new $18 million campus opened in May 2019, with a 50,000-square feet building that houses 244 students from 5 to 18.
“We eliminated or significantly reduced exposures to six major classes of chemicals,” Barnes said, including a group of “forever chemicals” known as PFAS. Plastic wrap can be used to cover food in plastic bowls. This can lead to the release of hormone-disrupting substances phthalates, bisphenol-A, and other harmful chemicals. Instead, it’s kept in stainless-steel bowls with lids made of medical-grade silicone. Teethers are made of natural rubber and not plastic.
Twelve million children five years old or younger are in child care in the United States. Barnes said she’s heard from parents, school administrators, and developers interested in replicating what the Children’s Enrichment Center created.
“We want to use this as a model for the early-childhood industry as a whole,” she said.
For the foreseeable near futureEvery year, thousands of children will be diagnosed with cancer and need treatment. They will be treated with less priority than adults unless the drug-development process undergoes significant changes.
Vickie Buenger, president-emeritus at the Foundation, stated that promising therapeutics for children face difficulties in moving from concept to commercial viability. Coalition Against Childhood CancerErin Buenger’s mother, who died in 2009 from neuroblastoma.

Erin Buenger.
“The children fall through the cracks because it’s tough to develop drugs for very small markets,” said Buenger, a business professor at Texas A&M University. She stated that although hundreds of cancer drugs have been approved by Food and Drug Administration, only six were created with children in view.
This disparity forces children to endure a “blast furnace of toxicity” during treatment with drugs designed for adults, she said. “They have to live with the side effects of such harsh treatment for decades.”
Agin, who stepped down from his law practice to run the nonprofit after Alexis’s death, stated that uplifting survival stories create a feeling of complacency. Max Cure FoundationLater, he started his own business. Prep4 Gold. “When the messaging is, ‘Look how great we’re doing,’ that drives the lack of haste in developing new therapies,” he said.
And survival doesn’t guarantee a normal life. Many childhood cancer patients develop new strains or have other health problems that are related to their treatments. Trevor Schaefer reported that he suffers from tinnitus, double vision, hearing loss and depression almost 20 years after his brain cancer diagnosis.
A National Cancer Institute spokesperson did not respond to written queries addressed to one of its pediatric experts. Instead, he mentioned a September blog postDr. Norman Sharpless, the institute director, praised the achievements. Sharpless noted that treatment methods have become more precise and result in better outcomes. Sharpless wrote that 90% of children with acute lymphoblastic Leukemia are now cured. It was nearly always fatal a half-century ago.
In response to the lobbying of the Coalition Against Childhood Cancer, and other groups, Congress tried to improve the odds of children with hard to treat tumors. It passed the Pediatric Research Equity ActIn 2003, the Creating Hope Act2011 and the Research to Accelerate Cures and Equity for Children Act2017 The bills incentivized, in varying degrees, drug discovery for pediatric cancers. But one loophole had been closed.
The legislation has shown “the beginnings of value,” Buenger said. After the bills were passed, all six FDA-approved child-focused oncology drugs were approved.
Gregory Reaman, a pediatric oncologist and associate director for oncology sciences at the FDA’s Center for Drug Evaluation and Research, cautioned that there are still “major challenges to cancer drug development in children because many of the cancers that are most difficult to treat and that remain as major problems from the standpoint of not having effective therapies are driven by molecular abnormalities that are very, very different from the molecular abnormalities that cause adult cancers.
“I think kids are at the back of the line because the laws have not allowed them to be at the front of the line, where they belong,” Reaman said. “So, that is now changing, and we’ll have to see if the change in the laws actually does live up to the promises…”
Peter Adamson, who leads cancer drug development at Sanofi, a global pharmaceutical company, said researchers’ understanding of childhood cancer has advanced, especially over the past decade, “and that understanding is now helping to drive research.”
Still, he said, cancer remains “the leading cause of death from disease” in children.
“I think the community continues to look for the right balance of requirements and incentives to help catalyze drug development,” Adamson said.
Buenger acknowledged the work of “good actors” in the private sector. Oncoheroes Biosciences Inc was one example of a company that was recognized in November. announcedIt had previously agreed to license volasertib to Notable Labs Inc. This drug is promising in treating acute myeloid and rhabdomyosarcoma. The drug will be available for children’s use, while the adult version will be available for adults.
But Buenger isn’t ready to declare victory.
“It’s a process, and we don’t want it to be just performative,’ she said. “We’re not going to be satisfied by people saying, ‘We’re trying.’”
Jim Morris is executive director of and editor-in chief of Public Health Watch,Non-profit investigative news organization. Lauren Berryman is a reporter for the Investigative Reporting Workshop, an independent, nonprofit newsroom based at American University’s School of Communication.